Augmented telemedicine is the forefront of digital health
Get to know one of knok’s main pillars and how it improves the quality of clinical decisions.
What is augmented telemedicine?
Improving the quality of clinical decisions, and presenting more in-depth medical insights and early diagnosis to name a few of the features Augmented Telemedicine offers. This concept – to elevate the potential of digital health – was originally designed to specify knok’s main pillars.
As the world population grows old by the minute, health organisations are facing a new health crisis: how to keep up with longer life expectancy? By living longer, people need more continuous care and treatment for complex health conditions that emerge during a later phase in life. According to WHO data and how medicine is continuously innovating, people over 60 will live longer and are expected to double in number by 2050.
This raises the question of how to deal with the costs of treating people that live longer, new medicines and procedures, which will inevitably cause a form of “healthcare inflation”. With the current market inflation and overall rising costs in distribution and logistics, other sectors have resorted to technology to improve their processes and increase efficiencies. Still, in the healthcare sector, technology adoption moves slowly.
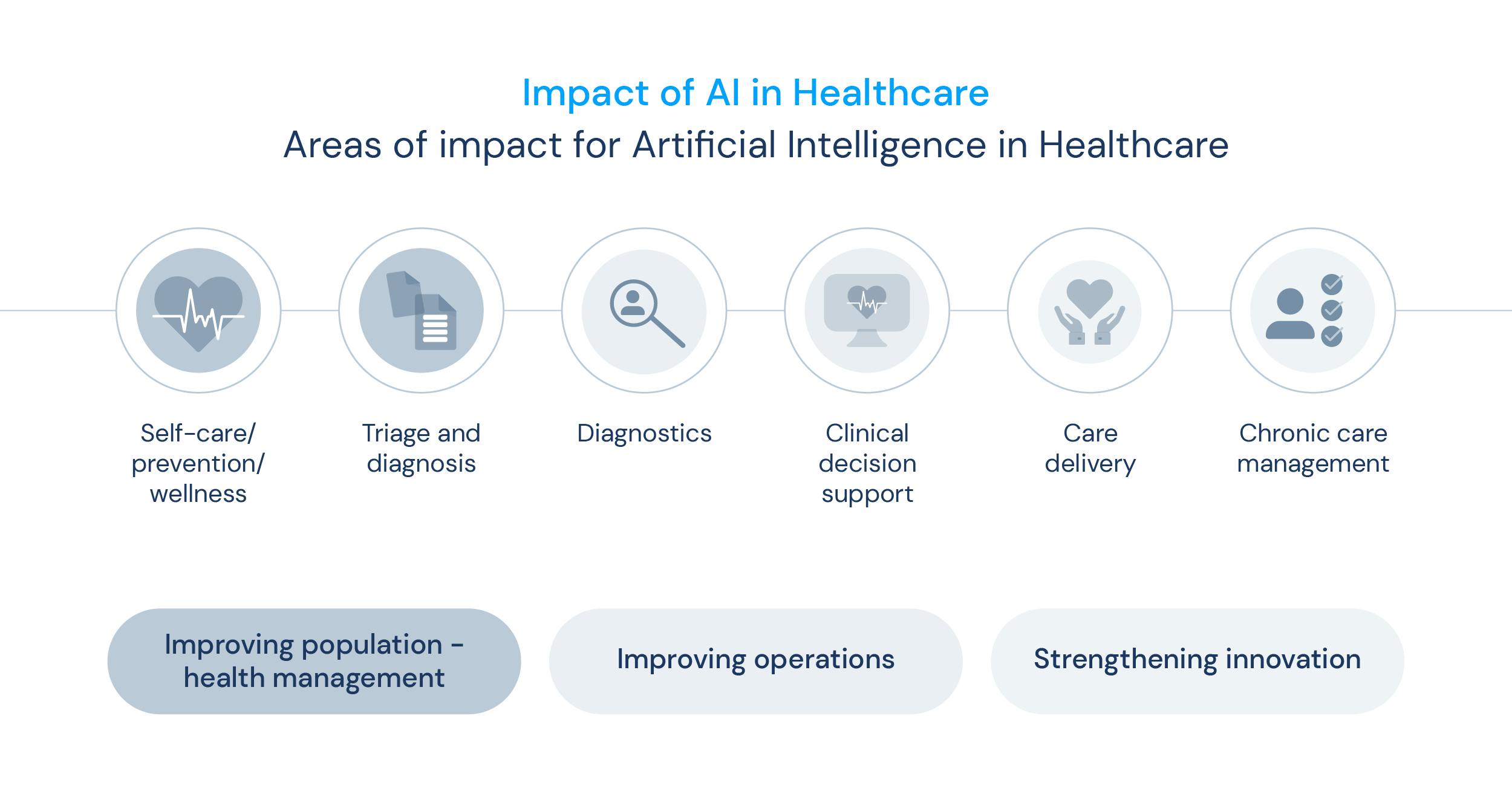
As Artificial Intelligence (AI) keeps growing among societal technology, it shows a promising application when using its features to better health processes and work-streams. These technologies make it possible to ease certain bureaucratic burdens for providers but also add value to businesses within healthcare such as health insurers. With machine learning advances, data can help predict behaviours and patterns in health status, which can constitute a major role in diagnosis. This embodies a concept of an elevated, augmented version of how to perform medicine.
Firstly coined by knok, augmented telemedicine is an AI-powered concept, a broader yet precise form of digital health. More than just regular health information doctors gather during consultations, augmented telemedicine is a remote medicine that uses data to empower doctors for better diagnosis and continuity of care to improve patients’ lives at a lower cost. But how does augmented telemedicine come to life, and how has it shaped the foundation for knok’s work? These are some key points we’ll dive deep into throughout this article.
How does augmented telemedicine come to life?
It's no doubt that healthcare systems worldwide need to shift their mindset and focus on healthcare that truly created value, but what is value in healthcare?
Ultimately, what adds and creates value in the healthcare sector are the patient outcomes and the correspondent accountability for resources in healthcare systems applied to that patient. Simply, this patient-centred concept focuses on improving the outcomes (how a patient is after treatment) and the costs spent to treat such intervention. The patient’s well-being is the focus for providers and an important variable when accounting for costs within healthcare industry.
A value-based care approach unifies patients, payors, providers, pharma and technology industries, policy and decision-makers with the same goal: improving patient outcomes, empowering and building accountability of providers as well as managing healthcare costs and bettering all-around efficiencies.

As mentioned before, augmented telemedicine uses AI that triages and reads vital signs by capturing data from connected devices patients use and tools that measure how they feel and by effortlessly recording lab analytics and other exams.
At knok, we believe AI, machine learning and data are powerful tools to be used in decision-making. In fact, with AT we give superpowers to doctors by empowering them with the strengths of digital health technology, and data-driven systems, getting closer and closer to a value-based care structure.
In a practical sense, augmented telemedicine helps healthcare providers and payors to develop specialised continuity of care programs based on knok’s verticals of care; these are the patient journeys designed for specific diseases and/or groups of patients, efficiently combining digital tools to improve clinical, operational and financial metrics. This scope breaks the constraints and barriers felt in a traditional telemedicine settings, in two different ways:
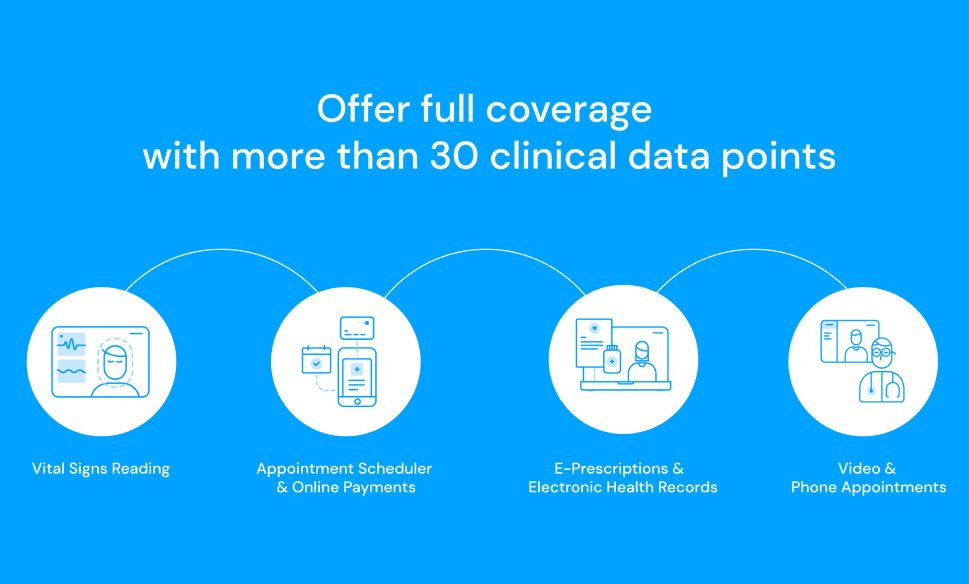
- collecting over 30 data points at every consultation;
- turning them into actionable data for practice:
- physicians who can make their diagnoses more efficiently and accurately,
- providers and payors who get a highly detailed and GDPR-compliant view of their customers.
This model originates from a quadruple winning formula of 4 P’s, where the success of knok’s model comes from Patients, Professionals, Providers and Payors.
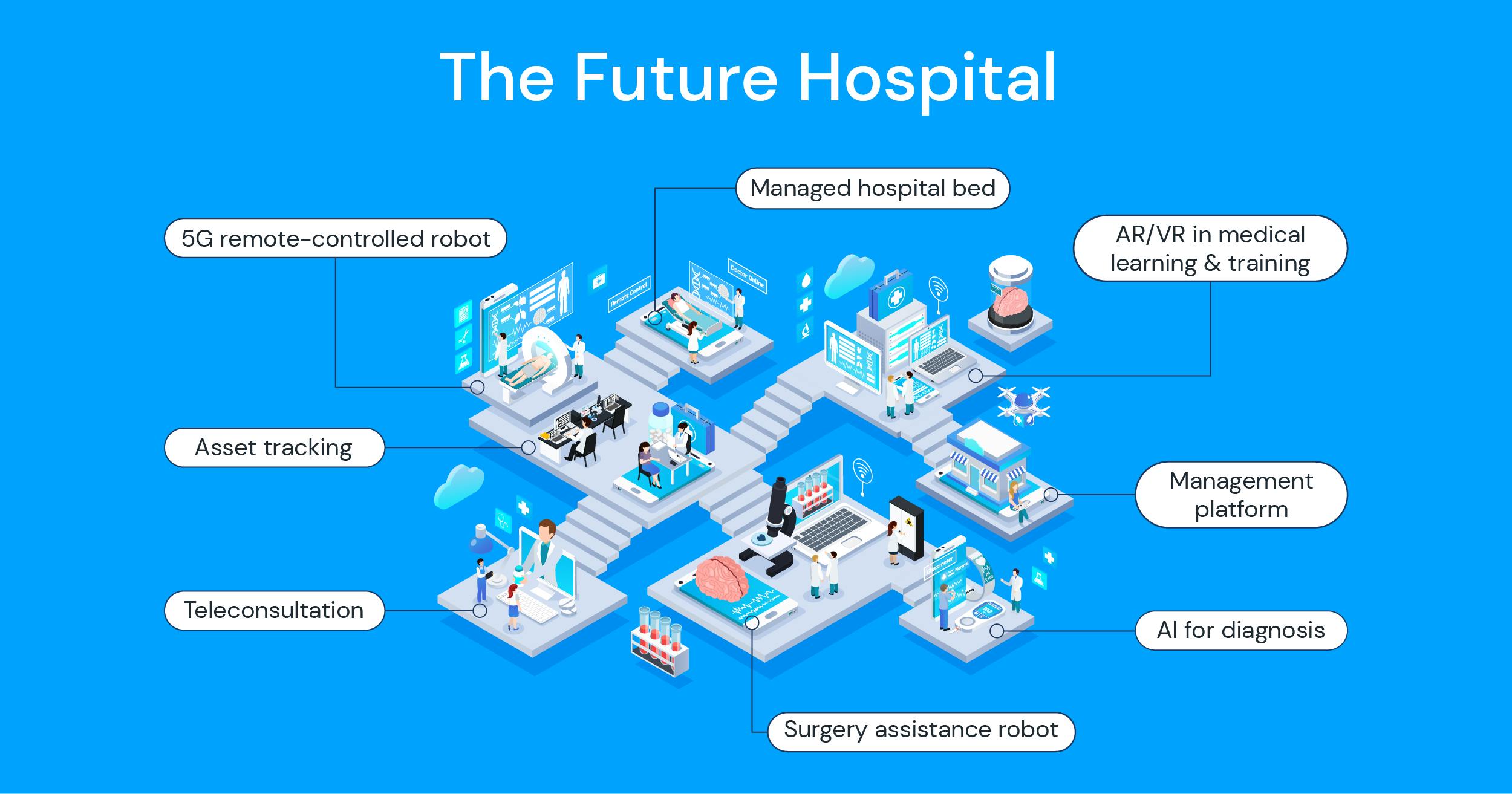
Augmented telemedicine for hospitals
By adopting AI in healthcare, we’re not substituting digital for analogue or manual labour. By acknowledging the power AI and digital health have to offer, we’re emphasising the Health in Healthcare! There are tons of insights that empower both doctors and patients: for doctors, being able to monitor patients without the paperwork and bureaucratic steps needed when in a hospital/clinical setting; and for the second, to keep track and have full ownership over their health status.
The technology behind these AI & Machine Learning solutions, along with the power of data collection, combines two important premises: prevent and predict!
It's important to humanise and prioritise healthcare literally, detaching from the conventional “disease care” - meaning prevention is key! Especially in the chronic conditions realm, prevention has proven its strength in reducing the risk of more serious sequelae and avoiding further episodes. When 52% of all adults have an underlying chronic disease, and most of them are preventable when monitored, this must be accounted for and boost the medical community to raise an action for it. On top of that, costs for treating chronic conditions and sequelae represent about 70% of healthcare costs in urgency rooms, which is a big number and needs to be cut down.
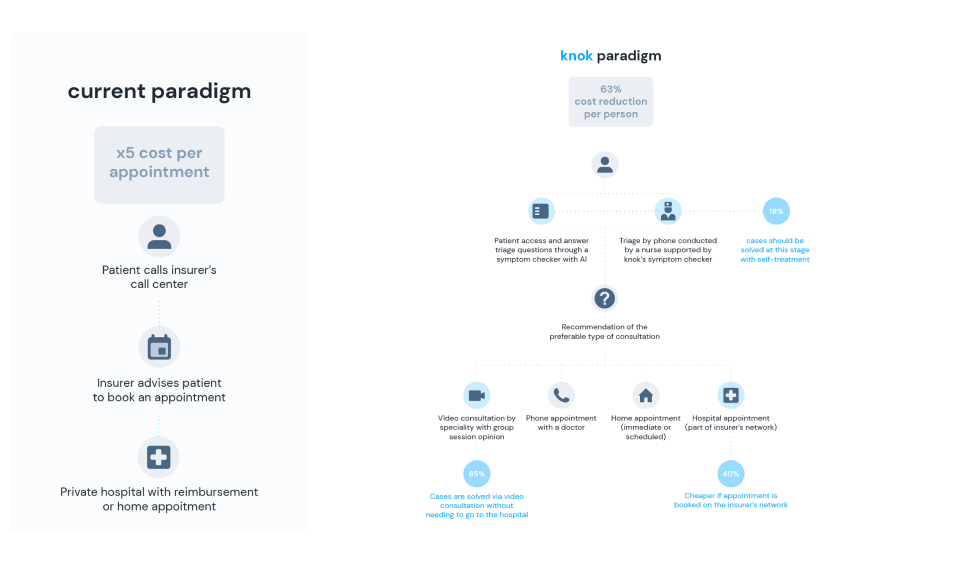
Other general benefits that improve efficiencies when adopting AI are triaging patients’ symptoms, for example, using a virtual triage symptom checker that redirects patients to the most appropriate level of healthcare according to their complaints, when research shows that about a fifth of UK visits to general practitioners and emergency rooms are related to minor problems that could be treated at home or with a simple virtual phone or video consultation. Considering the savings that could grow from freeing up emergency rooms (ERs) and unburdening triages, it’s believed that AI (in this sense) can become the first point of contact for healthcare systems.
Augmented telemedicine for health insurers
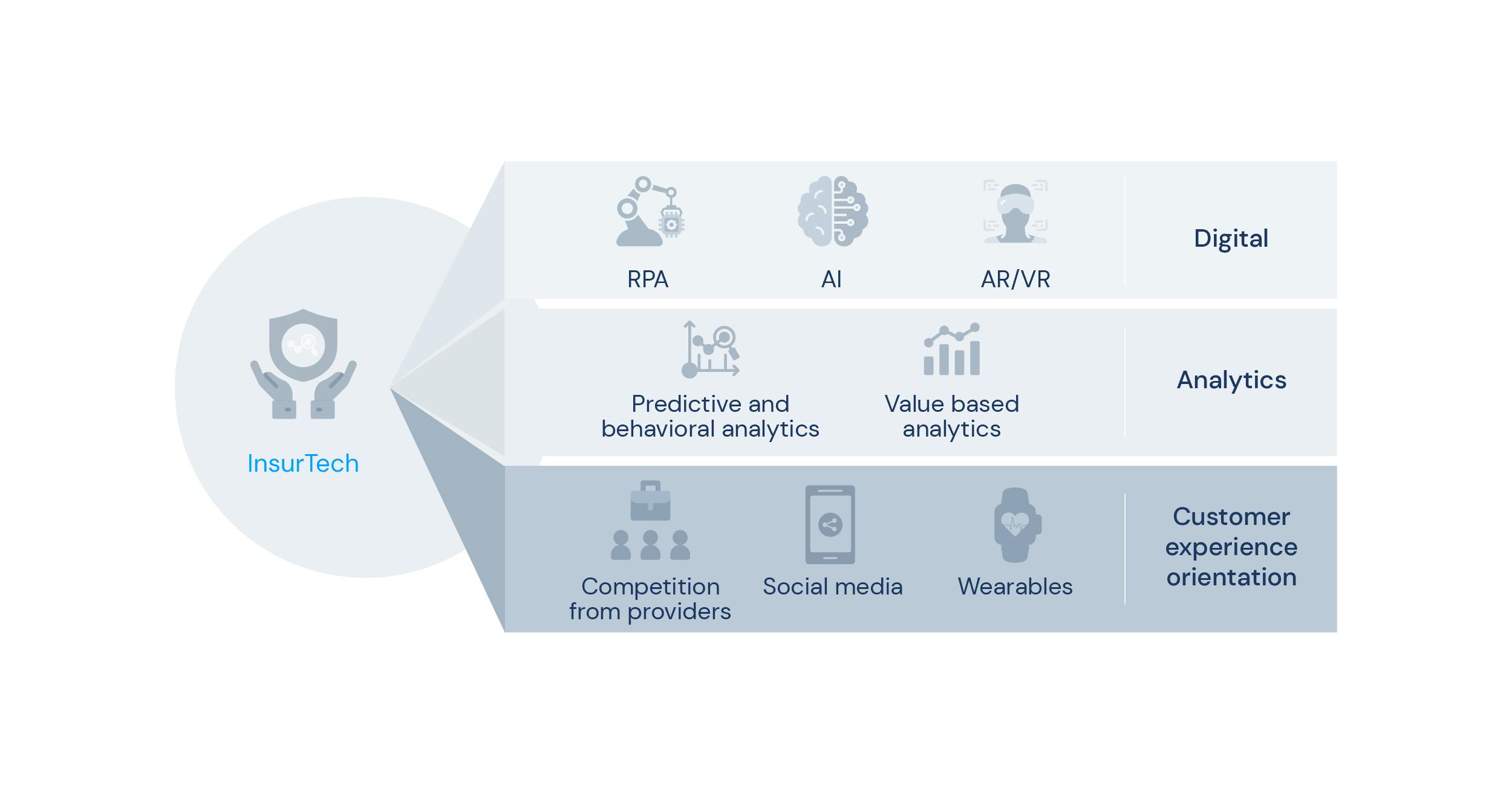
Across the many stakeholders healthcare resides, innovation resonates the most for health insurers since automation and having machine learning aids is a variable than estimates a cost reduction while improving efficiency and overall healthcare sustainability within health companies. While all seems to hit all the right points, where’s the applicability of Augmented telemedicine in a payors’ environment?
By having an approach to perception, data interpretation and prediction calculation, insurers will be able to automate certain tasks and create health clusters.
Using a fully anonymous data collection framework, these health status clusters show relevant clinical insights that can design personalised programs for businesses or tailor a specific segment within health companies. Prevention is knok’s middle name, and this data-driven model focuses heavily on avoiding a “sick-care” approach. Among others, we designed and implemented mental health Telemedicine programmes for young adults, general health Telemedicine programmes for elderly patients, and cardiovascular disease prevention programmes for hypertension.
Providers and patients
To acknowledge what value in a value-based care system means is a crucial aspect when shaping a structure. The defining aspect of value-based healthcare (VBC) is the fact that it seeks to tackle issues experienced in healthcare systems worldwide by emphasising on the single main objective that all stakeholders share: providing value to the patient by focusing on their outcomes. A patient-centred approach focuses on improving results and cutting costs for proposed population segments that receive segment-specific interventions, but true value-based care is more than improving numbers: it’s integrating patient care with quality outcomes and providing autonomy and accountability to providers to pursue the best way to deliver healthcare for the money spent.
For providers, the main benefit of this value-based model is enhancing motivation and lowering the workforce burden by reducing noise in work-stream processes, wasteful and admin tasks, and unnecessary interventions that (usually) are quite expensive. Looking back into the general costs spent in treating chronic diseases sequelae instead of investing in their prevention and continuity of care, adopting a VBC model would be a win for every party involved and would also address how care can be fragmented, consolidating everything.
Apps, Devices and Services
In some places in the world, having the possibility to reach difficult areas, or give patients the ability to attend their regular consultations without the distance factor, is an innovative solution; with Augmented telemedicine, we can have more than the regular telemedicine system. Adding to the data analysis and usage component, Augmented telemedicine can use medical devices and wearables to monitor patients, help build a digital platform to manage clinical teams, with synchronous (video) and asynchronous (chat and EHR) tools to communicate with every player involved.
Also, the wearable technology industry, like smartwatches and bracelets, is already spread out, with many uses available such as monitoring fitness and physical health, showing us all its potential as a great tool in the transformation of healthcare. Obviously, acknowledging its’ infancy stage and therefore not yet ready to to be used in daily healthcare reporting, such as to monitor various conditions, including a patient’s quality of life such as their physical intake during the day or cardiac response. Using a baseball analogy, we are only in “the third inning, there’s still a lot of ballgame to be played” even though all these factors have demonstrated great potential in providing data to spot problems early on, making life better for patients and saving healthcare systems money.
Augmented telemedicine and digital health
2023 has just started and the evolution within the digital health industry is clear: digital-first is here to improve our lives. As with every project or innovative technology, evolution, failure, and development are all parts of the process. Digital health is not a stagnant concept: it’s continuously being improved.
When combining the state of art science with the technology solutions of today, medicine entered its digital and virtual era, with the development of innovative digital solutions that better the traditional patient journey. With the mandatory stay-at-home policies during the COVID-19 pandemic, the acceptance of digital journeys became more mundane and, from patients to healthcare providers, the idea keeps growing (slowly) on people.
When talking solutions, one that aligns with physicians, hospitals but also stakeholders in health systems, we think of a solution that creates an easy, insightful and improved patient journey; and that’s where knok’s Augmented telemedicine comes in. By creating the right patient journey, designed specifically for each chronic disease or targeted population, we can change how healthcare providers their platforms to their patients and, consequently, improve their health all around.
knok 's Augmented Telemedicine as an essential steppingstone to gathering health data from devices, educating, predicting, and changing patient behaviours; this (of course) coming from a digital-first solution.
- But what’s the real scope of digital health?
- How does it differ from “traditional” analogue health today?
- How’s the digital health market and the stakeholders?
Introducing digital health
Innovation and technology are two important pillars for the evolution of today’s society and as inevitable as it can be, the presence of the digital world came to the healthcare sector. In a broader sense of the grammatical meaning, digital health englobes many categories such as:
- health information technology (HIT)
- mobile health (mHealth)
- wearable and smart devices
- telehealth and telemedicine
- personalised medicine.
Digital health technologies use machine learning, computing software and platforms for health-related purposes, being physical applications, medical products, and services. As mentioned before on Augmented telemedicine, the broader concept of digital health and digital-first solutions brings great potential in improving diagnosis, treat diseases and conditions, as well as enhancing the care in healthcare for everyone in society.
What to expect for digital health in 2023
Nowadays, it’s easy to understand the digitisation of healthcare with all available solutions, some being already used in daily tasks within the sector. Telehealth, EHRs (electronic health records) or online portals, are a just few already widely spread within hospitals and clinics; but what is the state-of-the-art in digital health technologies in 2023? What are the trends to look for?
One of the main features - and possibly also the downside - in the digital world is the rapidness of how something comes and goes. Looking at the latest most trending topic in business world, it’s only natural that it progresses to the healthcare sector. And yes, we’re talking about AI. While studies suggest the application of artificial intelligence can perform just as well or even better than humans in certain situations, it’s going to take a tremendous number of years before AI can replace human technical tasks in the medical field. So how can AI be used today, and what’s expected of the future of digital health technologies?
Let’s explore these applications.
The applications of digital health technologies
Since we’re living in a post-pandemic scenario, adding the inflation bubble, workforce issues, on-going corporate burnout and many other concerning matters of our society, there’s a big margin for uncertainty on what to expect from healthcare. Organisations, payors, and digital health companies must align their strategies in order to not only supply the needs for individuals when searching for healthcare, but also convey the confidence and be aware of the urgency of innovation in the sector.
- Artificial Intelligence is the way
With the growing popularity of machine learning and artificial intelligence, and the latest cutting-edge sensation ChatGPT, the possibilities begin to arise. The real value here is using these technologies to aid in diagnosis and treatment, analysing big data, creating predictive models and unburden administrative tasks. The practical usage have been proven, the carpet is laid down for digital health companies to walk on.
- Value-based care will be the new continuous care
There’s no denying on how telehealth and telemedicine can improve efficiencies in regular patient journeys. Many medical conditions and acute situations can be solved within a virtual care setting, avoiding going to an ER or medical centre. The increasing usage of digital-first solutions enable remote patient monitoring (RPM) solutions, which increase convenience, access, and efficiency. This resonates with a primary care virtual model, which is aligned with the motto: prevention is key!
- Primary care will enable digital health technologies
As mentioned in the previous point, transforming parts of the healthcare system into digital, strengthens work-streams, provides higher quality of care, better outcomes at lower costs and overall, better patient experience. In a recent report from the National Academies of Sciences, Engineering, and Medicine, “primary care is the only healthcare component where an increased supply is associated with better population health and more equitable outcomes” – which emphasises the need to invest and take part in bettering systems using digital solutions. The usage of these solutions can automate clerical functions and reduce the workload of primary care physicians. Efficient digital health systems can also aid in decision-making processes and furthermore, take action; create and integrated care model that delivers across communities and be more equitable and of high quality.
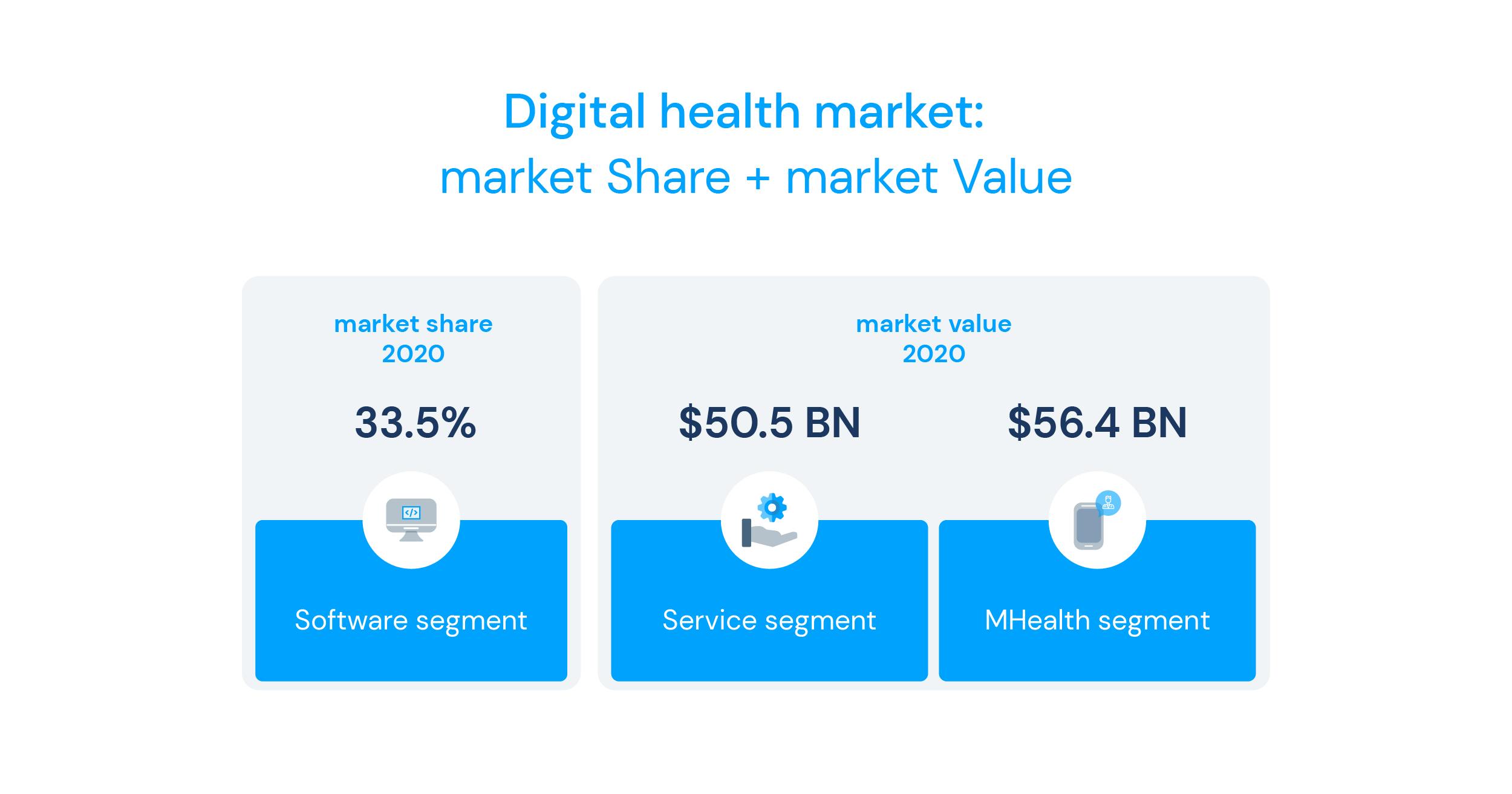
Digital health perspective in the insurance market
Segmenting the market based on the technology, the global market is divided into digital health systems, healthcare analytics, telemedicine, and mobile health. The most growing demand comes from telemedicine services which have regenerated around 41.56% of the segmental revenue. This growing demand for managing and monitoring healthcare data along with other factors like people management in real-time, data security and privacy, and all related secure storage of healthcare-related information is leading the demand for telemedicine services.
This paves the way for the concept of Augmented telemedicine to take its place in healthcare systems but also in patient-driven models. This convergence of high technology with healthcare creates efficiencies across the continuum of care and enhances the power of innovation. Providing patients with more liberated access to their health journey, easing processes and workloads for providers, and breaking inefficiencies for stakeholders is the utopic dream in the digital and smart health world. These insights are major when setting up and developing healthcare solutions, but also reshape how we view health in general and pave the way to a new relationship between patients, healthcare providers and health systems in general.